What is the problem?
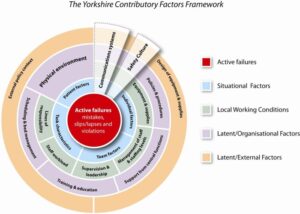
 Racialised incivilities are subtle, everyday acts of disrespect, exclusion, and hostility which are a common but overlooked experience in NHS maternity services. While the NHS promotes equality, diversity, and inclusion, racially minoritised staff remain unfairly exposed to unprofessional behaviours such as incivility, bullying, harassment and abuse (from multiple sources) that harm their wellbeing, teamwork, and pose a risk to patient safety (Keller et al., 2020; Woodhead et al., 2021). These behaviours are often minimised as personality clashes or communication issues, meaning the racialised nature of harm is rarely recognised or addressed. Current safety frameworks focus on systems and individual error but largely ignore how structural inequity and discrimination shape workplace cultures, behaviours and care quality (Schulson et al., 2022; Maben et al., 2023).
Racialised incivilities are subtle, everyday acts of disrespect, exclusion, and hostility which are a common but overlooked experience in NHS maternity services. While the NHS promotes equality, diversity, and inclusion, racially minoritised staff remain unfairly exposed to unprofessional behaviours such as incivility, bullying, harassment and abuse (from multiple sources) that harm their wellbeing, teamwork, and pose a risk to patient safety (Keller et al., 2020; Woodhead et al., 2021). These behaviours are often minimised as personality clashes or communication issues, meaning the racialised nature of harm is rarely recognised or addressed. Current safety frameworks focus on systems and individual error but largely ignore how structural inequity and discrimination shape workplace cultures, behaviours and care quality (Schulson et al., 2022; Maben et al., 2023).
Why does it need to be addressed now?
The NHS faces growing workforce pressures and rising reports of discrimination with 86% of NHS Trusts reporting disproportionate exposure of unprofessional behaviours for racially minoritised staff. Without targeted action, the emotional exhaustion and disengagement caused by racialised incivility will continue to undermine staff retention, morale, and the quality and safety of patient care. Existing “listening” systems, such as Freedom to Speak Up, Human Resources and Organisational Development, often lack the racial literacy and sensitivity needed to capture or respond effectively to subtle forms of harm.
What difference will it make?
Addressing racialised incivility is both a moral and clinical imperative. This PhD helped to identify mechanisms and patterns of incivility within a racialised organisation, unearthing the link between uncivil behaviours and their multilevel consequences. The findings highlighted incivility in routine work practices, social interactions and management practices, which illuminates targets for future intervention development. In maternal care, where teamwork and timing save lives, incivility compromised information flow, created delays and disrupted safety preparedness, that threatens care to mothers and babies. The informal and formal listening roles and associated structures, which aimed to support and alleviate these negative behaviours, were often subject to and complicit in minimising incivility experiences and impacts. In addition to their limited resources and poorer decision making influences for change. Embedding equity into safety culture through anti-racism frameworks, compassionate and accountable leadership with structured longer-term evaluation, and better-designed reporting systems can improve staff wellbeing, strengthen teamwork, and enhance patient safety. Tackling these everyday inequities will help create fairer, psychologically safer workplaces and contribute to more inclusive, high-quality maternity care for all.
You can download a visual summary of the PhD here


 Racialised incivilities are subtle, everyday acts of disrespect, exclusion, and hostility which are a common but overlooked experience in NHS maternity services. While the NHS promotes equality, diversity, and inclusion, racially minoritised staff remain unfairly exposed to unprofessional behaviours such as incivility, bullying, harassment and abuse (from multiple sources) that harm their wellbeing, teamwork, and pose a risk to patient safety (Keller et al., 2020; Woodhead et al., 2021). These behaviours are often minimised as personality clashes or communication issues, meaning the racialised nature of harm is rarely recognised or addressed. Current safety frameworks focus on systems and individual error but largely ignore how structural inequity and discrimination shape workplace cultures, behaviours and care quality (Schulson et al., 2022; Maben et al., 2023).
Racialised incivilities are subtle, everyday acts of disrespect, exclusion, and hostility which are a common but overlooked experience in NHS maternity services. While the NHS promotes equality, diversity, and inclusion, racially minoritised staff remain unfairly exposed to unprofessional behaviours such as incivility, bullying, harassment and abuse (from multiple sources) that harm their wellbeing, teamwork, and pose a risk to patient safety (Keller et al., 2020; Woodhead et al., 2021). These behaviours are often minimised as personality clashes or communication issues, meaning the racialised nature of harm is rarely recognised or addressed. Current safety frameworks focus on systems and individual error but largely ignore how structural inequity and discrimination shape workplace cultures, behaviours and care quality (Schulson et al., 2022; Maben et al., 2023).

 What is the problem?
What is the problem?