Led by Professor Rebecca Lawton and Professor Beth Fylan
Martha’s Rule is a new patient safety initiative being piloted by NHS England. Martha’s Rule gives all NHS inpatients, their carers and NHS ward staff the right to an independent clinical review of a patient’s condition whenever they feel that themselves or a loved one/patient is deteriorating, but they don’t feel that their concerns are being taken seriously by the immediate ward staff looking after them. It also requires ward staff to obtain information relating to a patient’s condition directly from patients and their families at least daily.
In June 2024, the implementation of Martha’s rule commenced in 143 NHS Trusts where 24/7 critical care outreach was in place. In the first instance, this will cover all inpatients in acute hospital trusts with the exception of maternity, neonatal and emergency department services. The first rollout of Martha’s Rule will also not include mental health or community services.
There is a strong moral imperative for Martha’s Rule and its potential to make significant improvements in patient care and outcomes. However, the evidence base for this initiative is limited and its implementation is likely to be challenging. Rapid implementation of such an initiative before it has been adequately tested could lead to unintended consequences such as diverting critical care resources and potentially increasing inequalities (Rae et al., 2018). Therefore, there are unanswered questions about the potential and actual impact of the implementation of Martha’s Rule for services, healthcare staff and patients/families.
Our formative evaluation will be evaluating the implementation phase of Martha’s Rule, understanding how the sites have operationalised Martha’s Rule and the factors that have helped or hindered how successful that process of implementation was. The research aims to address a number of research questions about the potential impact of the first phase of implementation/rollout of Martha’s Rule for services, healthcare staff and patients/families as well as factors that contribute to successful implementation.
We aim to use the outcomes of this evaluation to produce a set of recommendations to inform;
- Future policy in this space
- National guidance for other trusts planning to implement Martha’s rule
- A full-scale summative evaluation of the implementation of Martha’s Rule which will be focussed on effectiveness.
For further information on this evaluation please see our FAQs.
If you have any further questions, please email marthasrule.study@bthft.nhs.uk.
Patients, family members and staff can visit our participant page for details on how to get involved in this reseach.
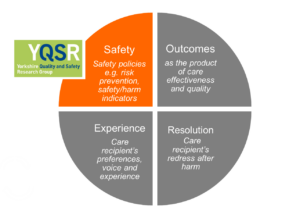 The Yorkshire Quality and Safety Research group (YQSR) has been appointed to deliver the patient safety arm of NIHR QSO PRU in collaboration with the universities of Oxford, Leeds, Bradford, and the Picker Institute.
The Yorkshire Quality and Safety Research group (YQSR) has been appointed to deliver the patient safety arm of NIHR QSO PRU in collaboration with the universities of Oxford, Leeds, Bradford, and the Picker Institute.





